Almost all of us at one time in our life have had an ankle sprain. In fact, according to American Academy of Orthopedic Surgeons, 25,000 people sprain their ankle each day! Although most ankle sprains are commonly self-diagnosed, if not treated properly, they can lead to repetitive ankle sprains causing further damage and chronic ankle instability.
What causes ankle sprains?
There are many factors that can lead to an ankle sprain, so it’s important to address each one and learn ways to prevent any possibility of future sprains. Many times, it is purely weak muscles and tendons across the ankle joint that lead to increased risk of lateral ankle sprains. Poor ankle flexibility due to tight muscles such as the gastrocnemius and soleus or lack of proper warm-ups can lead to an increased risk. Poor joint proprioception and lax ligaments from prior ankle injuries can further increase the risk for lateral ankle sprains. Lastly, improper shoe wear and running on uneven surfaces play a significant role in lateral ankle sprains.
Different Grade Ankle Sprains
 ankle diagram image - Courtesy of Beantown Physio
ankle diagram image - Courtesy of Beantown PhysioOnce an ankle sprain occurs, it is important to know how significant the sprain is to determine how long it will take to heal and rehabilitate it to its fullest potential. There are three main ligaments that support the lateral ankle: anterior talofibular ligament, posterior talofibular ligament, and calcaneofibular ligament. When describing an ankle sprain, they are classified as grade I, II, or III, depending on the amount of damage to the ligaments of the ankle. With a grade I sprain, there is some damage to the ligament, but the stability of the ankle is not compromised. With a grade II sprain, there is a partial tear of a ligament, causing some instability. And, with a grade III sprain, there is a complete tear of one of the ligaments, causing significant instability, bruising, and swelling. While NSAIDs and ice help to alleviate the swelling and pain, strengthening and proprioceptive exercises are needed to help strengthen the ankle and prevent future injury or trauma to the ankle.
Rehabilitation:
If there is a significant amount of swelling, bruising, and instability, it’s best to see a MD or Physical Therapist (PT) to determine the severity of the ankle sprain and/or perform a differential diagnosis.
If it is determined to be an ankle sprain, a suggested rehab program would be as follows:

Weeks 0-1
Minimize swelling: STM (soft tissue massage), ice, compression, elevation, electrical
Stimulation
Gentle ankle mobilizations to restore joint movement (done by a PT)
Ankle range of motion exercises: alphabet, seated towel stretch (Fig 1a), standing calf stretch (Fig 1b-c), and stationary bike without resistance.
Strengthen joints above: Knee and hip strengthening exercises: (PT to determine where there are muscle imbalances)
Aquatic therapy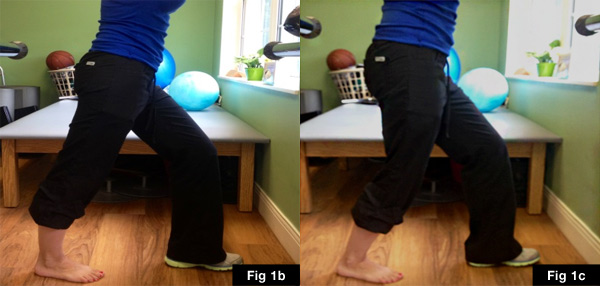
Taping for Stabilization: During the first few weeks of rehab, it is important to help stabilize the ankle to minimize stress on the joint, ligaments, and tendons. For the first week, the tape should be worn at all times for stabilization purposes and to decrease the stress put on the lateral ankle. After 2-3 weeks, the tape can be worn during workouts and runs. Although there are several different taping techniques, I prefer a particular taping technique using kinesiotape. (See video)

 Weeks 1-3
Weeks 1-3
Continue with ankle mobilizations, ankle range of motion (ROM) exercises, and RICE (rest , ice, compression, elevation)
Add seated and standing calf raises, leg press, leg curls, total gym, sitting on therapeutic ball with balance exercises.
Add theraband ankle exercises with focus on dorsiflexion, plantarflexion (Fig 2a) and eversion (Fig 2b)
If pain-free by the end of week 2-3 and bruising and swelling have diminished, begin light jogging with kinesiotape to ankle to prevent lateral stress on the ankle. Although the ankle may be pain-free, it has not fully healed at this time, and it is important to protect the ankle from further damage
Weeks 4-8
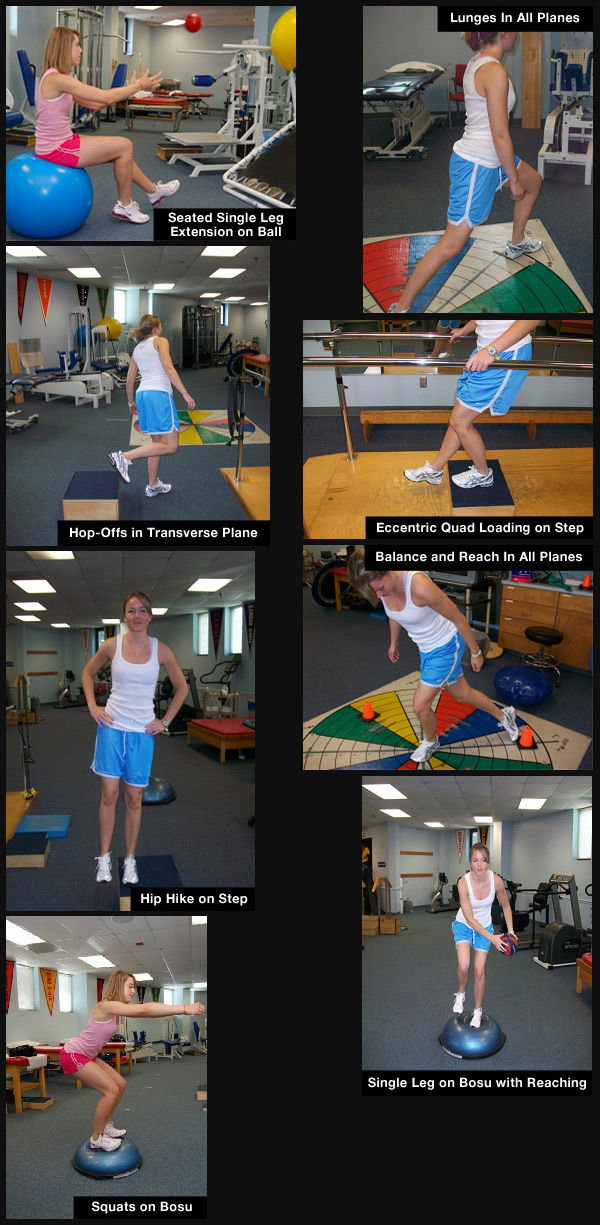
Proprioceptive retraining and bilateral lower extremity exercises progressing to single leg stability exercises are important in this phase to improve balance and strengthen the muscles around the ankle. Since ligaments are avascular, they do not repair the damage, they simply develop scar tissue. Thus, it is important to learn stabilization exercises for the ankle to prevent future ankle sprains.
See pictures below:
The above mentioned is just a guideline, healing time varies from person to person. Thus, it is important to not rush the healing process and to take the appropriate amount of time to rehabilitate the ankle and prevent chronic ankle instability.
Works Cited
“Sprained Ankle-OrthoInfo-AAOS. “Sprained Ankle-OrthoInfo-AAOS. American Academy of Orthopaedic Surgeons, Sept. 2012. Web. 20 Aug. 2013.
This article and/or product are not intended to provide medical advice, diagnosis or treatment.
 This article was written by Melinda Branch, DPT – VPX Team Xtreme OCR Athlete. Melinda has a bachelor's degree in dietetics and attended the University of Kansas Medical Center to obtain her Doctorate of Physical Therapy.
This article was written by Melinda Branch, DPT – VPX Team Xtreme OCR Athlete. Melinda has a bachelor's degree in dietetics and attended the University of Kansas Medical Center to obtain her Doctorate of Physical Therapy.